Homelessness and Healthcare
Health costs of Homelessness in Seattle
February 5, 2020
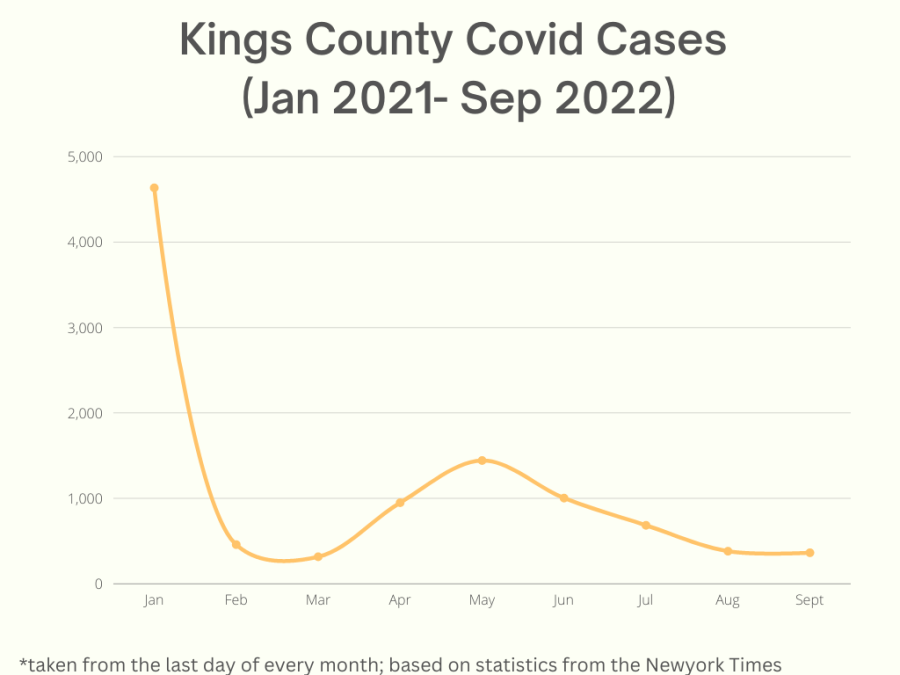
Since Seattle declared a state of emergency around homelessness in 2015, the homeless population has only continued to age — and with that comes a slew of health problems that homeless shelters are not prepared to deal with. In the 196 deaths of presumed homeless individuals in King County during 2018, the largest category of 38% was that of “natural causes,” and 59% of all presumed homeless deaths were those of individuals above the age of 50, according to the King County Health Examiner.
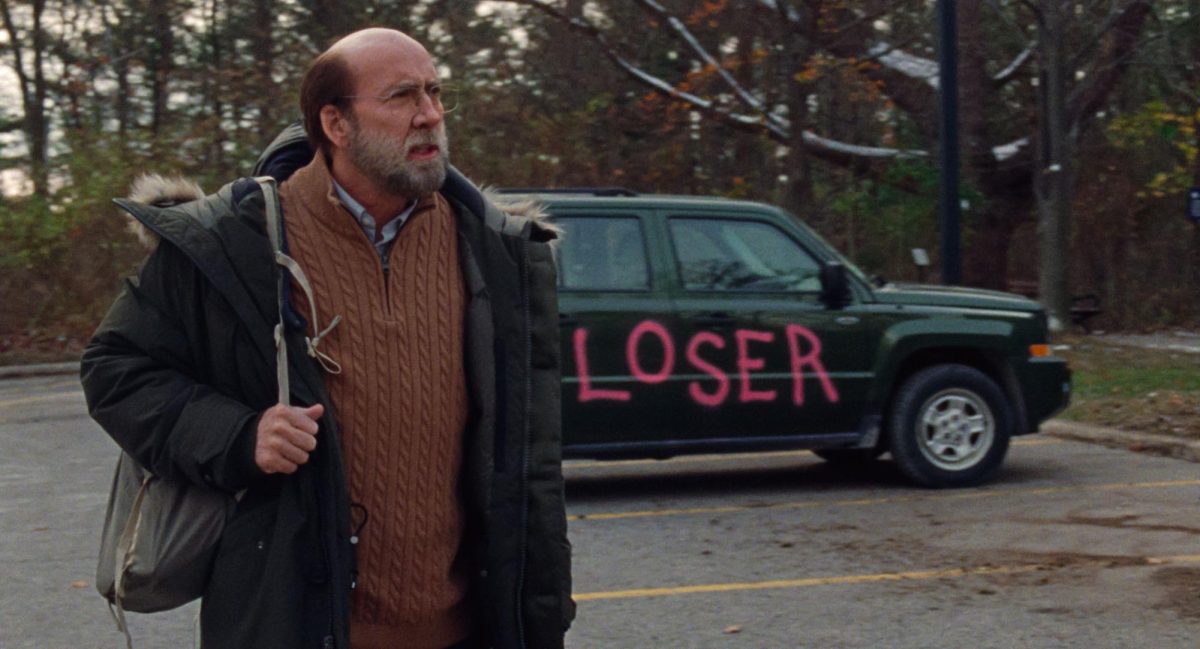
Mental illness and substance abuse are the reasons many assume that Seattle’s homeless population, already large, continues to grow. Largely ignored populations of the chronically homeless — those who have been homeless for over a year or who have been homeless several individual times — are physical disabilities and diseases, which for many have caused or perpetuated their state of homelessness.
People who live in shelters in the United States are twice as likely to have a disability than the general population, and health threats such as heart disease and HIV/AIDS are far more prevalent among the homeless. There are multiple, intertwined reasons for this: the main one, of course, being poverty, and the unclean situations in which poverty places people that often transmit illnesses.
Diseases considered easy to treat, or at the very least keep at bay in the general population, are made incredibly more difficult to treat by housing instability. Diabetes, for example, is considered manageable for many. But for a homeless or housing insecure individual, syringes may be stolen, proper places to store refrigerated insulin may be inaccessible and diets in homeless shelters are not typically suited towards particular health restrictions.
Already understaffed and underpaying homeless shelters rarely have medical professionals on their teams and sometimes even lack room for oxygen tanks or electrical outlets for proper medical equipment.
Medical care can be difficult to access for the many homeless individuals who lack insurance. While Seattle hospitals are required to treat anyone regardless of their ability to pay, discharging people who do not have a place to stay makes for a difficult ethical decision: either discharge homeless patients, or take in patients that can pay up.
Some cheaper options for homeless outpatient care are available, offering prices of $400 a night as opposed to a hospital’s $2,000 a night bill, but this payment is still far too high to demand from the chronically ill and homeless community.
While many of these elderly and homeless individuals impacted by disability or disease may be good candidates for senior-care facilities, state regulations declare that these programs are at risk of losing their accreditation if a client dies of overdose. This means that many senior-care facilities will refuse to take in homeless clients, not due to a lack of insurance, but because of the rate of substance abuse in the homeless community.
This causes obvious issues: Given that homeless shelters cannot afford to treat the myriad of illnesses suffered by their clients, these homeless individuals are obviously being physically hurt and incapacitated by their diseases. However, the progression of a debilitating illness only perpetuates the inability to get treatment.
If an individual struggles with mobility, sight or breathing, this creates difficulty for them to get a job, even if they might have a stable shelter in which they are able to live. This clearly detrimental cycle is a major reason for homelessness across the globe, given that many homeless individuals cite either the initial loss of a job or the perpetual inability to get a job as the main reason that they are homeless.
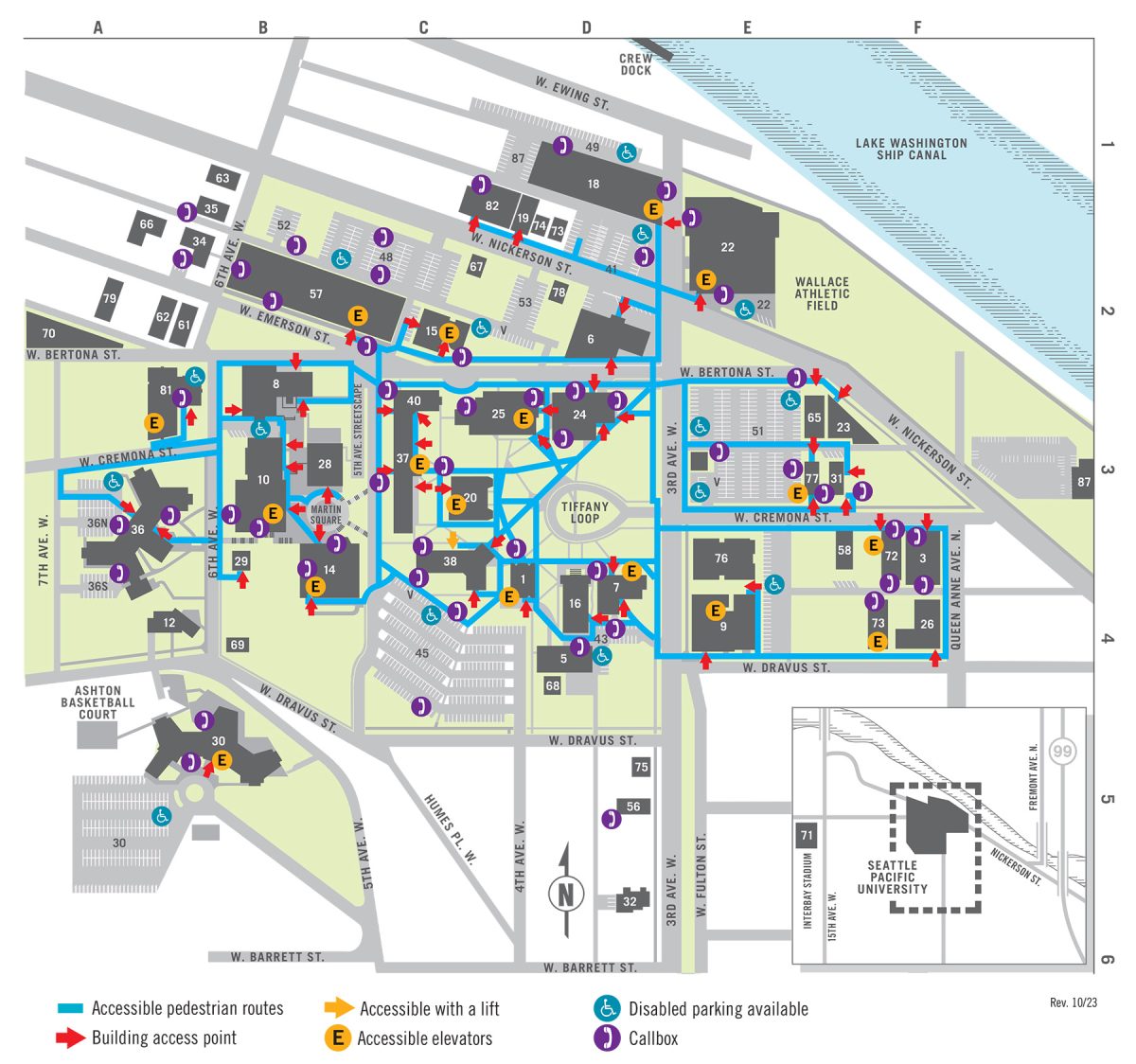
Seattle’s Healthcare for the Homeless Network (HCHN) is taking steps to solve this issue, with public care centers, mobile care units and some free clinics for children and teens. But when a persistently homeless individual with a chronic illness is treated in a one-time scenario and released back onto the street, the cycle is simply going to repeat itself. The homeless community, particularly those suffering from illnesses, need stable housing and reliable healthcare to recover.
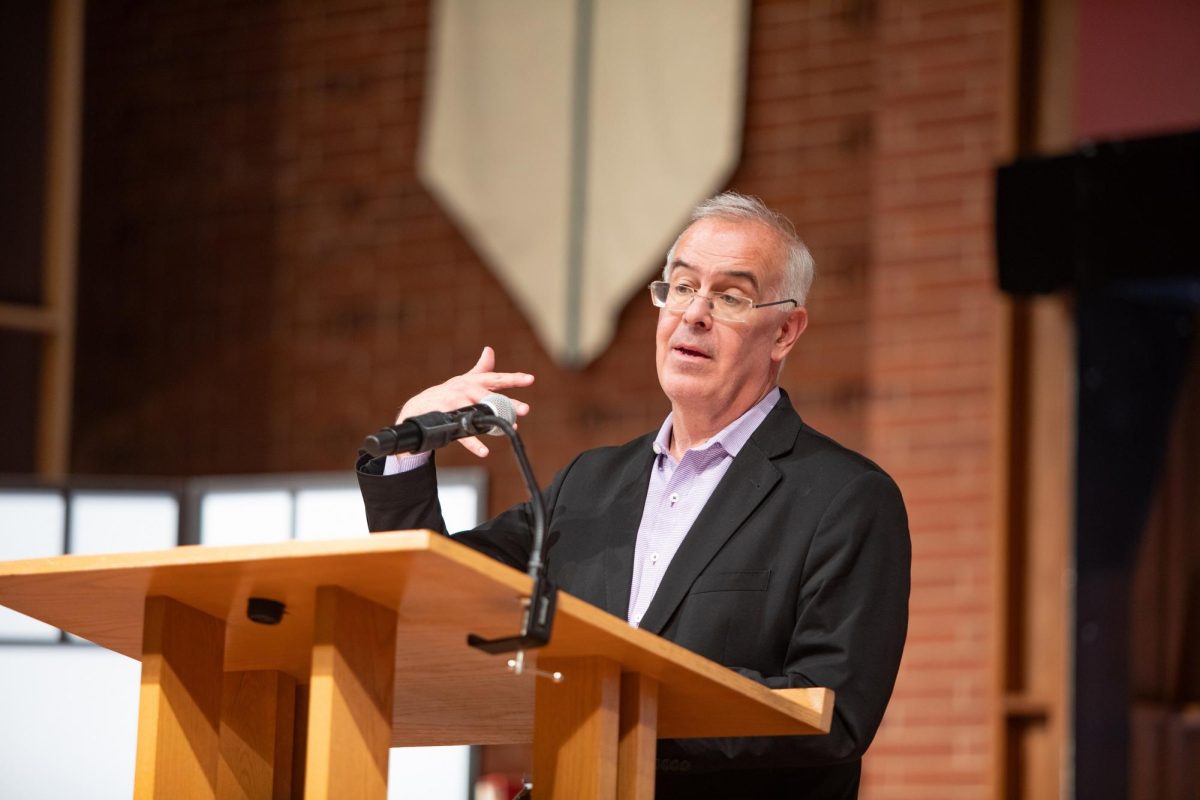
At Washington state’s legislative session in January, Jay Inslee proposed a bill that would spend $300 million over the next three years toward supporting permanent housing, food support and enhanced shelters in an attempt to cut Washington’s unsheltered homeless population in half.
“I believe we have an obligation to help solve the problem,” he announced. “Our compassion will not allow us to look the other way.”