Discussing mental health alongside a faith perspective requires an integration that is responsible, consistent and honors multiple areas of study, according to Lauren Dudugjian, a graduate student at SPU pursuing a double-major in marriage and family therapy and a masters of divinity.
“Often, issues of mental health get wrapped up and repackaged in spiritualized language; our theology is wrapped up into it and can be used as a simplified tool of oppression of each other,” Dudugjian said. “It’s not necessarily that we’re seeing theology being used to beat people down, it’s that we’re seeing wounded people pick up something beautiful, but it gets wrapped up in our own brokenness and we then hurt each other with it.”
That is why NAMI at SPU, the SPU chapter of the National Alliance for Mental Illness, hosted a panel discussion titled, “The Intersection of Faith and Mental Illness” Tuesday afternoon in Weter 202: to discuss ways in which faith perspectives can be both compatible with mental health issues and also problematic at times.
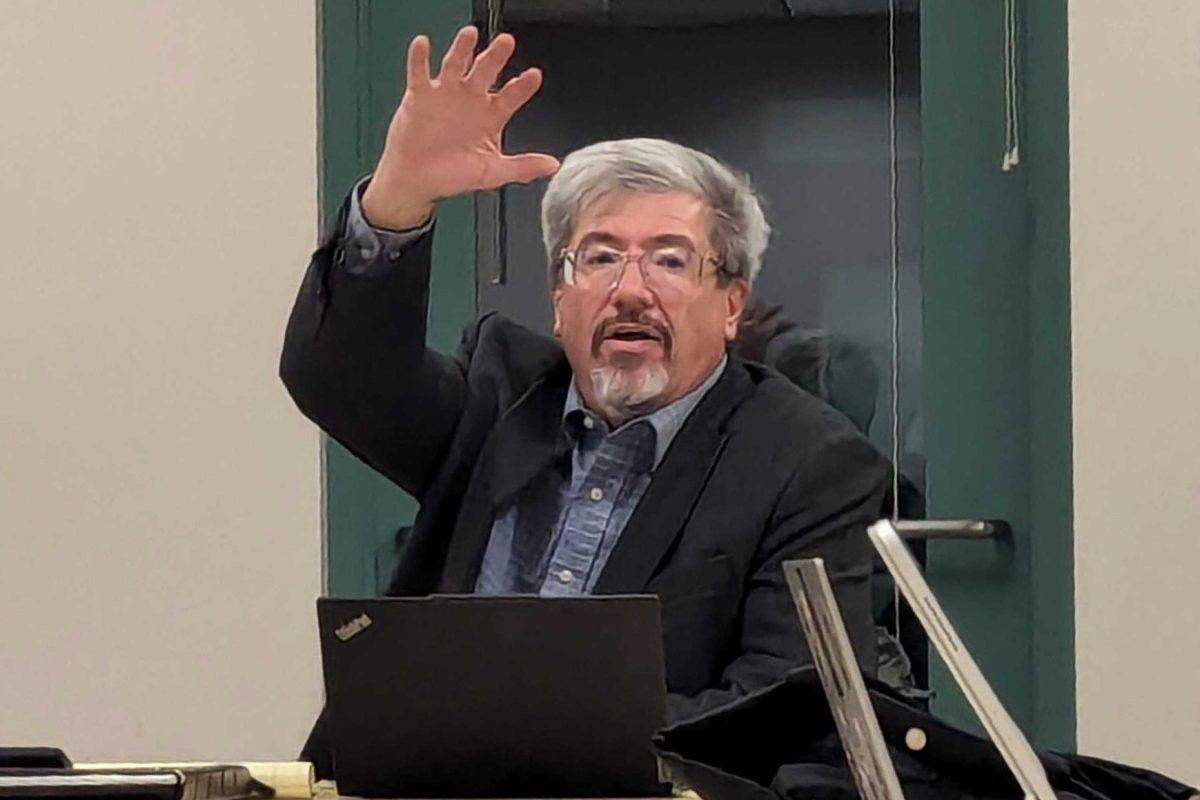
In addition to Dudugjian, the panel included Phil Maulding, a licensed counselor and the pastor of congregational life at Bethany Community Church; Sadie Teal, a doctoral student in SPU’s department of clinical psychology and a counselor in SPU’s counseling center; and David Nienhuis, SPU professor of New Testament studies.
Speaking from personal experience, NAMI at SPU President Jessi Morris believes that religious institutions have failed many folks struggling with mental illness, making it hard for them to reconcile their struggle with their faith.
NAMI at SPU is made of up of Morris, a junior studying psychology; Candice Xia, a senior studying nursing; and Maria Niño and Sarah-Ann Moh, both seniors studying psychology.
These four students are the undergraduate recipients of the Dickinson Fellowship, a component of SPU’s Living Well Initiative that supports NAMI at SPU.
In addition to providing education and access to resources, Morris says the goal of NAMI at SPU is to reduce the stigma surrounding mental illness by talking about it.
“We want to just let people who are on campus who are struggling know that people hear you and other people know that you are here at this school,” Morris said. “Just know that you are cared about and we are working to educate the school about this.”
For Dudugjian, a graduate recipient of the Dickinson Fellowship, the bias to see faith and mental health as incompatible is an ironic one.
“The irony is that the scientific revolution came out of the convictions of faith somewhat, and so these things were meant to be integrated,” Dudugjian said. “I don’t have to disregard the things I’m seeing in the world scientifically because of my faith or vice versa. When I see things that don’t make sense it’s not a signal to throw something out but rather to press forward. I ask how I can grow in my understanding.”
Moving forward in churches, Dudugjian sees a need for people who are going to pay attention to the mental health strengths and issues at play, to ask where their community needs to grow and how they are going to transform their theology to be something that is more redemptive and healing rather than an either/or situation.
While prayer, participating in a faith community and being in relationship with God have neurological impacts, Dudugjian says it does not mean faith is collapsable to biochemical mechanisms.
“To over-spiritualize or under-spiritualize these issues is to not be scientific and empirical with what you are seeing,” Dudugjian said. “It just means you are dealing with both [faith and mental health].”
Maulding identified a problem with over-spiritualizing mental illness, seeing the conditions as something that can be prayed away.
“Yes, God, I believe, can divinely heal us, mentally, physically, but he also has given us many gifts and one of those gifts is the gift of modern science and medical help,” he said. “To say that his healing does not come through modern medicine is just a falsehood.”
Drawing from NAMI’s 2015 study that indicates approximately one in five adults in the U.S. as experiencing mental illness in a given year, Maulding identified transparency about these occurrences as a major struggle for religious institutions in regard to mental health.
Maulding finds it ridiculous that a physical ailment warrants further observation, inspection and diagnosis while a mental illness is often dismissed.
“For some reason we can spiritualize it and call it a secret sin, which drives me crazy,” he said. “It’s such bad theology to see sin in mental illness.”
From Nienhuis’ experience, it’s rare to find churches that incorporate people struggling with mental illness as a normative part of the whole self that people bring to worship.
“The fact that we can’t see God operating through medicine and through doctors is really an indictment against the way we’ve conceived of theology in the West for a long time,” Nienhuis said, “as though there is this radical separation between individual and community or between body and spirit. All this is symptoms of the radical distortion that has gone on for such a long time, and we’re only just now starting to climb